
The current study evaluates of the effect of 360-degree laser on the rate of SSAS following primary PPV with or without SB for RRD. However, studies that have looked at its use in primary PPV for RRD have yielded conflicting results. Theoretically, application of 360-degree laser creates a chorioretinal scar that may wall off subretinal fluid conduits from anterior to posterior retinal areas and cover any missed breaks. One method proposed to reduce re-detachment rates in patients undergoing PPV is 360-degree prophylactic endolaser photocoagulation. Missed retinal breaks, new retinal break formation, opening of old retinal breaks and proliferative vitreoretinopathy have been identified as major causes of retinal re-detachment. Single surgery anatomical success (SSAS) is a key outcome in primary RRD repair as the risk of recurrent detachment and poor functional outcome increases with subsequent procedures.
Disadvantages include the risk of new retinal breaks, cataract formation and elevation of intraocular pressure. The major advantage of PPV is the potential for improved visualisation of the retinal periphery, allowing increased identification of retinal breaks. However, PPV continues to increase in popularity as a first-line procedure. Traditionally, SB was considered the procedure of choice for primary RRD. Techniques in use include pneumatic retinopexy (PR), pars plana vitrectomy (PPV), scleral buckling (SB) and combination PPV and SB. Successful surgical management of RRD requires effective treatment of retinal breaks and relief of vitreoretinal traction.

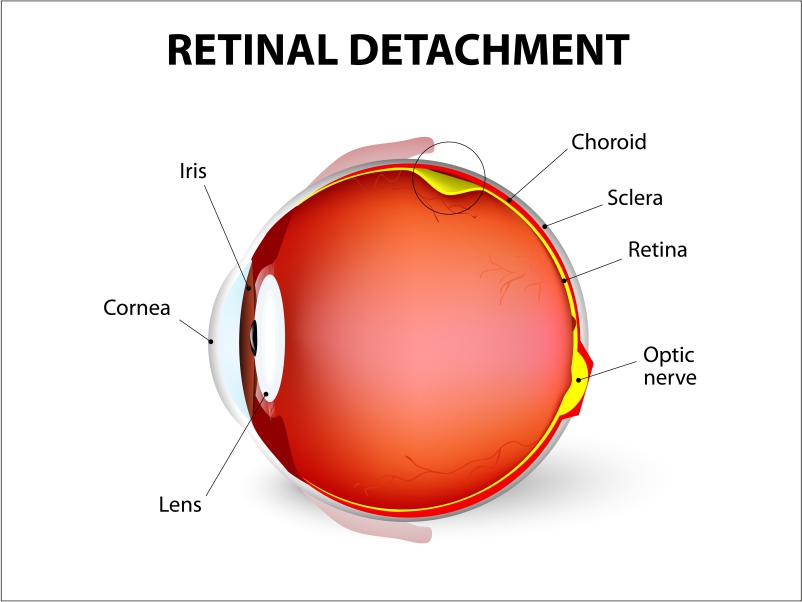
Therefore, timely and successful treatment of RRD is crucial for improved visual prognosis. This can lead to significant visual morbidity, particularly if there is extension into the macula. As a consequence of the neurosensory retina separating from the retinal pigment epithelium (RPE), the outer retina loses its choroidal blood supply and becomes ischaemic. Rhegmatogenous retinal detachment (RRD) is a vision-threatening condition caused by tractional forces of the vitreous onto the retina leading to full-thickness retinal tears and accumulation of fluid in the subretinal space. Even when accounting for this, there was no difference in surgical outcomes or complication rates. Conclusionsģ60-degree laser retinopexy during primary PPV ± SB for RRD was associated with more complex cases and more extensive operations. Worse preoperative logMAR visual acuity (P = 0.009), male sex (P = 0.060), higher PVR grades, supplemental SB (P = 0.0468) and silicone oil/C 3F 8 tamponade (P 0.9999) or corneal epithelial defects (P = N/A) were found. The study included 192 cases, of which 130 received 360-degree laser. Multiple logistic regression and multivariate regression was used. Secondary outcomes included visual acuity, epiretinal membrane formation, the presence of cystoid macular oedema, tonic pupil and corneal epithelial defects. The primary outcome was single surgery anatomical success (SSAS). Patients who underwent PPV ± SB for repair of non-complex RRD at a single centre were included in this retrospective study.

To determine patient and surgical factors associated with the use of 360-degree laser retinopexy during primary pars plana vitrectomy (PPV) ± scleral buckle (SB) for rhegmatogenous retinal detachment (RRD) and its impact on surgical outcomes.


 0 kommentar(er)
0 kommentar(er)
